Moderate exercise to boost immune function has been at the forefront of exercise recommendations during the Sars-CoV-2 pandemic. In this piece I will identify the most common athletic concerns & what to do if you had COVID before return to sport. The immunologic benefits of moderate exercise, and conversely the potential for increasing inflammation and infection risk with more intense and sustained exertion, have driven recommendations. With a bit of daylight in diminishing cases shining through our sports medicine windows, we begin to plan the re-entry to sport with considerations to protect the heart.

Athletic participation has had a complete pause for most Americans in the weeks following the cancellation of the NCAA tournament. Like dominoes, every major sporting organization subsequently suspended competition and training. A major concern for all athletes is reconditioning by establishing exercise routines to support re-entry. Cardiovascular fitness is the foundation of performance science. Here I will explore some considerations that you and your organizations should bear in mind as you gear up for the return to sports.
What to do if you have NOT had a recent COVID infection and feel fine:
Deconditioning is the primary concern athletes will face as sports participation begins. It is important to address this first with use of a fitness schedule that supports cardiovascular exercise. While it is tempting to try to pick up where you left off, starting slowly and rebuilding can help to prevent injury. Utilizing a heart rate monitor, you can methodically begin exercise and progress exertion and duration objectively. A daily symptoms journal to accompany exercise recordings can identify trends in soreness that are heading toward injury.
Also, it is possible that people may have had exposure to the novel coronavirus without significant symptoms. If symptoms such as shortness of breath, fatigue, or chest pain occur, further evaluation with your doctor should commence immediately. Commonly, people that have recovered from even mild infections will note recurrence of cough & decreased exercise capacity upon reinitiation of exercise. I will cover lung considerations in another post. In any event, if symptoms occur, consult your physician.
If you had COVID disease:
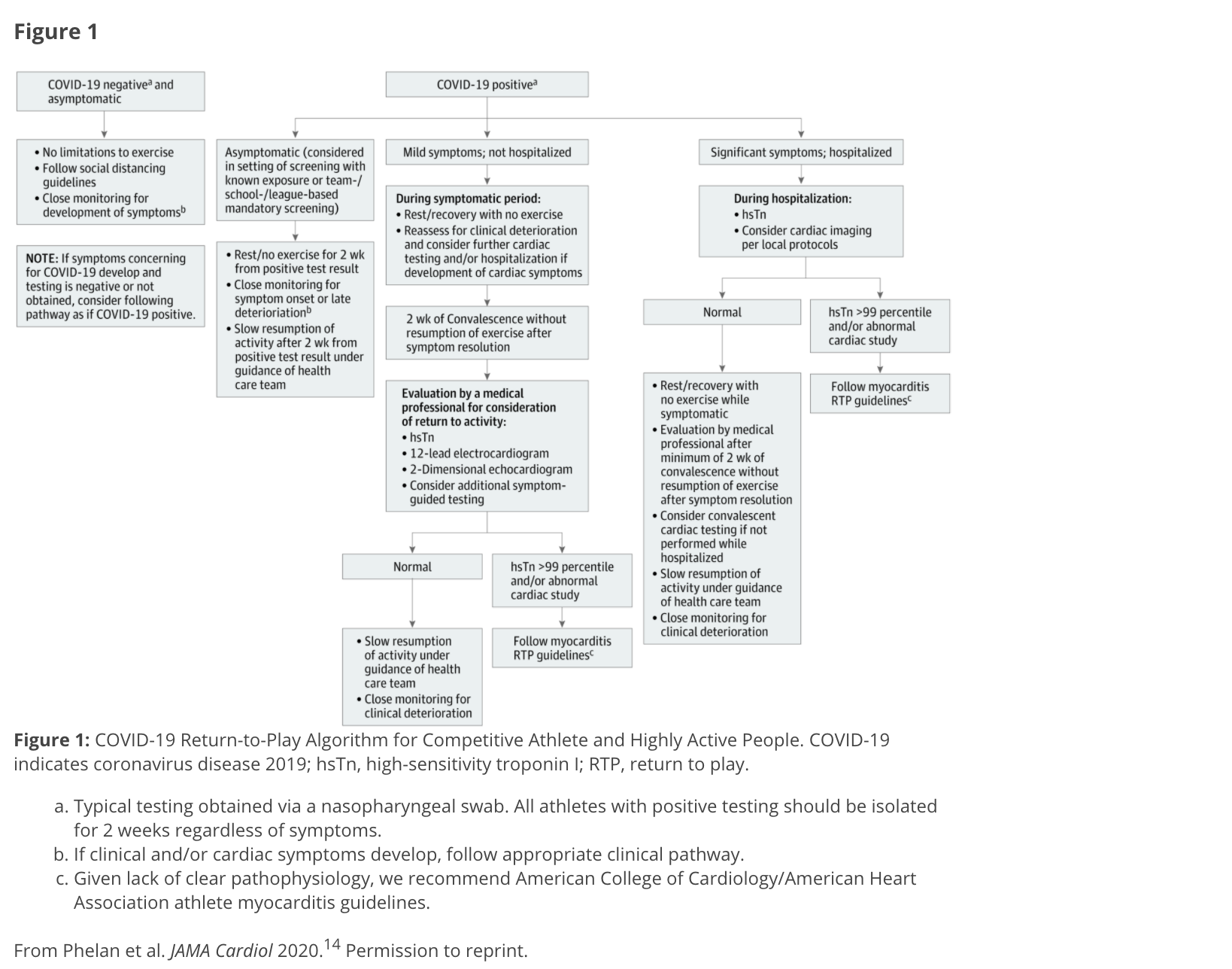
For many healthy, young adults and adolescents, COVID causes a mild-moderate respiratory illness that does not require hospitalization. Exercise during an active infection is never a good idea and can lead to permanent damage to the heart or even death. That being said, SARS-CoV-2 infection is known to include the additional risk of an infection of the heart. Exercise should follow a waiting period (after complete recovery) of at least 2 weeks in mild cases and for competitive athletes with known cardiac involvement, 3-6 months as currently recommended by expert consensus. In any event, an evaluation with your sports doctor prior to initiation of exercise is important given the lack of knowledge regarding the impact of this disease in the short & long term.
Because the virus can attach to the angiotensin receptor, there is a direct risk to the entire cardiovascular system. Specifically, the virus can cause myocarditis. Symptoms of this disease might include shortness of breath & chest pain, or this can be a silent (asymptomatic) infection of the heart. Sudden Cardiac Death (SCD) is a concern for competitive sports, and this is a risk for which we screen most athletes at the collegiate level & elite athletes each preseason. After an active infection with coronavirus we are recommending athletes consult with their sports doctor for evaluation and consideration for further testing prior to heavy exertional training, live practices, and sport.
The following figure from the recent consensus statement from the American College of Cardiology provides guidance for evaluation.
Return to sport considerations for individuals and teams:
For recreational athletes some common sense guidelines should be employed. Physical distance (6 feet) while exercising is important. More vigorous exercise should prompt increased distance from others as the potential for droplets to travel further with running and biking has been suggested in studies. Currently, exercising with a mask on is not recommended, but having a face covering handy for times at which proximity to others is unavoidable can help diminish the risk of infection from asymptomatic carriers.
Organizations and teams must have policies in place regarding cardiac clearance prior to return to sport. While pre-participation requirements are relaxed at this time due to potential obstacles in access, athletes known to have had infection should not participate until appropriate evaluation and work up is completed. Suspected cases and contacts of those infected must be tested with appropriate isolation from the team according to isolation policies.
In the absence of active infection, coaches must be aware of the risk of injury, including cardiac concerns. A methodical progression is essential and foundational training must happen over the course of 3 weeks or more. Again, heart rate monitoring can be a vital tool in identifying fatigue and guiding progression of training.
Conclusion:
As the data increase over time recommendations for COVID-19 treatment and follow up will certainly evolve as well. All individuals should eliminate exercise if there is concern for any viral syndrome, especially when febrile. In cases of myocarditis or other cardiac injury, a waiting period of 3-6 months before re-entry to vigorous exercise is recommended.
- COVID-19 is a respiratory infection with the potential to cross into systemic circulation and cause multiorgan dysfunction, including cardiac disease.
- Cardiac screening including ECG, troponin levels, & echocardiogram are recommended after COVID-19, even if only mild illness occurs.
- Viral infections can cause myocarditis. Never exercise during an acute illness.
- Myocarditis can occur with other viral infection, but in particular SARS-CoV-2, which can increase sudden cardiac death (SCD) risk by up to 20%.
_____________________________________________________________________________________

Leave a reply to lineecas Cancel reply